Our intelligent ventilation mode turns you from a knob-turner into a supervisor. INTELLiVENT-ASV reduces the number of manual interactions with the ventilator (
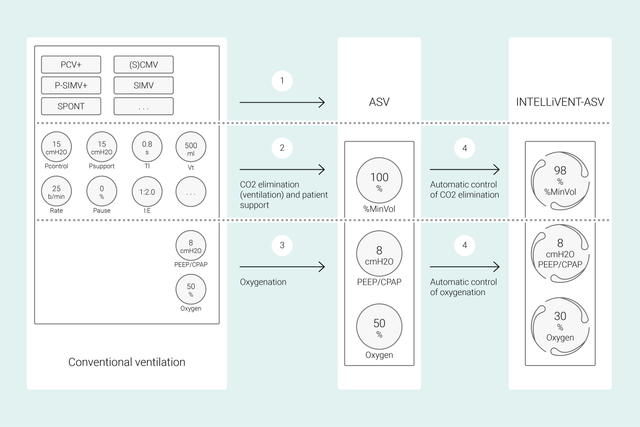
In conventional modes, you set multiple ventilator controls such as tidal volume or pressure, respiratory rate, FiO2, PEEP, and expiratory and inspiratory time to achieve certain clinical targets. Additionally, all these controls need frequent reassessment and adjustment.
With INTELLiVENT‑ASV, your defined clinical targets and strategies for oxygenation and ventilation are the central focus. Once you have set these targets, you can decide to what extent INTELLiVENT‑ASV should control oxygenation and ventilation in order to achieve them.
INTELLiVENT‑ASV then automatically selects ventilator settings, manages the transition between passive and active states, and actively supports your weaning protocols using Quick Wean.
Multiple international studies have demonstrated the safety and performance of INTELLiVENT-ASV in various clinical scenarios - from post-cardiac surgery (


In this video, Dr. Jean-Michel Arnal, Senior Intensivist, gives you a quick demonstration of the main functionalities and settings in INTELLiVENT-ASV on a real ICU patient.
At the beginning, you set the patient's height, gender, and, if necessary, specific condition: ARDS, chronic hypercapnia, or brain injury. Next, you set the clinical targets in terms of oxygenation (SpO2) and CO2 elimination (PetCO2) for your patient.
You then have various options to fine‑tune INTELLiVENT‑ASV. For example, you can decide whether you want to set PEEP manually or if you want INTELLiVENT‑ASV to set PEEP within a range defined by you. After reviewing or setting alarm limits, you are ready to start ventilation.
INTELLiVENT‑ASV implements your strategy at the bedside. Instead of making frequent changes to individual settings, you monitor and readjust the targets and strategy when necessary.
INTELLiVENT-ASV aims to bring the patient into your defined target range and keep them there ‑ while maintaining lung‑protective ventilation (
These inputs are measured by three sensors: The proximal flow sensor provides data on lung mechanics and patient activity, while the SpO2 and CO2 sensors provide data on oxygenation and CO2 elimination.
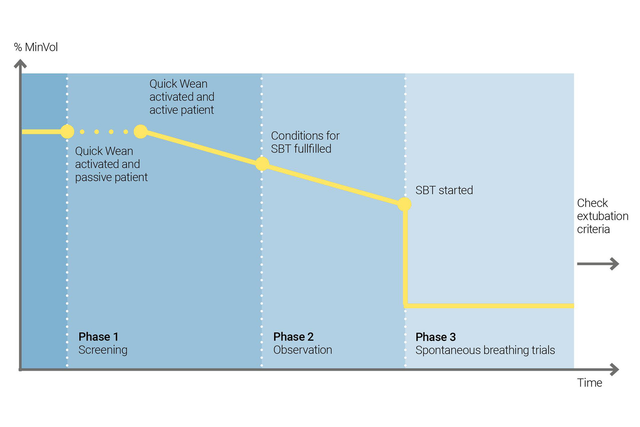
Use INTELLiVENT‑ASV's Quick Wean to implement your weaning protocol. You can enable Quick Wean during ventilation when the patient is breathing spontaneously.
You can configure Quick Wean by enabling SBT to evaluate your patient's readiness to be separated from the ventilator. You adjust the criteria for starting an SBT, the settings to be used while the SBT is running, and the criteria for aborting it.
INTELLiVENT‑ASV always displays the history of all performed SBTs. If an SBT is unsuccessful, INTELLiVENT‑ASV reverts to the previous ventilation settings.
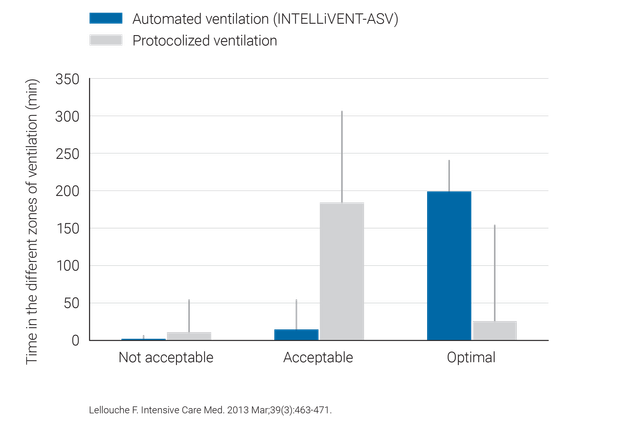
Clinical studies have shown that INTELLiVENT‑ASV selects safe driving pressure (
INTELLiVENT‑ASV requires fewer manual adjustments than conventional ventilation and thus supports in lowering the workload for the healthcare team (

INTELLiVENT-ASV is available as an option on the HAMILTON-C6, HAMILTON-G5, HAMILTON-C3, HAMILTON-C1 and HAMILTON-T1, and as a standard mode on the HAMILTON-S1.