
作者: Caroline Brown, Giorgio Iotti
日期: 08.07.2022
在机械通气的病人中,病人和呼吸机之间的不同步现象很常见 (1, 2)。

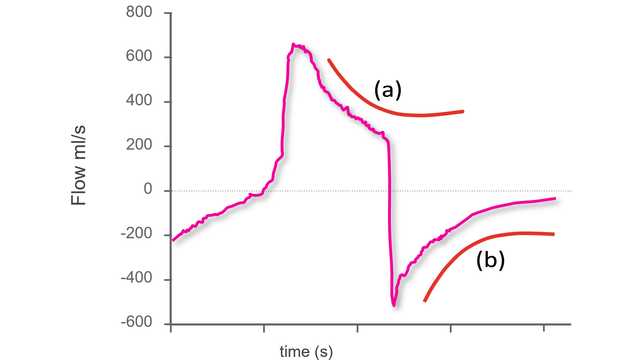
病人和呼吸机的吸气和呼气时间之间的这种不匹配可能采取各种形式(如提早或较晚切换、自动触发、双重触发或无效努力),并已被证明会影响病人治疗效果 (
分析气道压力和流量波形以检测呼吸努力及其时间的概念在近三十年前首次被描述 (
该试验的一个关键要素是使用系统方法分析气道压力和流量波形,该方法包括五个一般生理原理和一组预先定义的特定规则(“波形法”)。所有病人均在压力支持模式下使用食道导管进行通气。该方法应用于使用近端传感器获得的气道压力和流量波形,并使用食道压 (Pes) 作为参考。对于每名病人,来自四人小组(三名高级医师和一名住院医生)的三名研究人员只分析了流量和压力波形,而另一名研究人员分析了流量和压力波形以及食道压跟踪。呼吸被分类为“正常”辅助、自动触发、双重触发或无效努力。在正常辅助呼吸的情况下,还评估了较小的不同步(触发延迟、提早切换和较晚切换)。
主要终点是使用波形法检测到的自发努力的百分比。次要终点包括波形和参考方法在检测较大和较小不同步方面的一致性,以及波形法的评价者之间的一致性。
共记录 4426 次呼吸。使用参考食道压测量,其中 77.8% 被确定为呼吸机正确检测到的呼吸,22.1% 被确定为无效呼吸,0.1% 被确定为自动触发呼吸。波形法能够检测到 99.5% 的自发努力和除一次外的所有自动触发呼吸。同样,将呼吸确定为辅助、自动触发、双重触发或无效的参考方法和波形法之间的一致性非常高。不同步指数——计算公式为自动触发、无效和双重触发呼吸的总和除以呼吸总次数——为 5.9%,使用波形法与食道压进行评估时没有差异。不同步总时间——计算公式为人机不同步的时间除以总记录时间——为 22.4%,其中较小的不同步占 92.1%。不同操作人员对呼吸分类的一致性也很高。
在 90% 以上的病例中,波形法使研究人员能够以足够的精确度识别呼吸努力的开始和结束,从而也可能正确识别“较小的”不同步——触发延迟、提早切换和较晚切换。
这项研究提出了一些重要的发现。研究人员表明,波形法使临床医生能够检测到极高比例的自发努力,并准确评估病人的活动时间。即使对于较小的不同步,波形法也是高度可靠和可重复的。该研究的进一步发现强调了这一点的重要性,即 PSV 中的大多数不同步时间与较小的不同步有关。
这些结果不仅证明了波形法的可重复性(操作人员之间的高度一致性);它们还显示,根据预定义的系统方法进行波形分析的训练起着关键作用。有证据表明,治疗机械通气病人的临床经验并不一定等同于识别不同步的能力,而 ICU 医生识别不同步的能力总体很低 (
作者得出结论,气道压力和气流的近端波形包括足够的信息来准确评估病人活动和人机交互,假设采用适当的系统分析方法,如“波形法”。
Hamilton Medical 哈美顿医疗公司呼吸机集成的 IntelliSync®+ 技术(
完整引文如下: (

我们的异步参考卡向您概述了最常见的异步性类型、它们的原因以及如何检测它们。
The first step to identifying asynchronies using standard ventilator waveforms is knowing what a synchronous breath looks like during pressure-support ventilation.
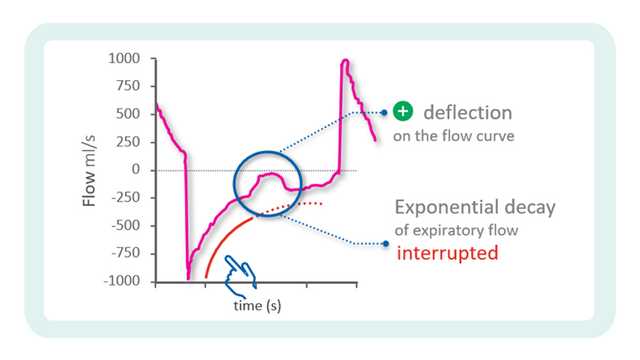
In the previous issue, our Bedside tip covered the starting point for identifying asynchronies using ventilator waveforms.