Благодаря интеллектуальному режиму вентиляции вам больше не нужно крутить рычаги. В режиме INTELLiVENT-ASV сокращается количество ручных взаимодействий с аппаратом ИВЛ (
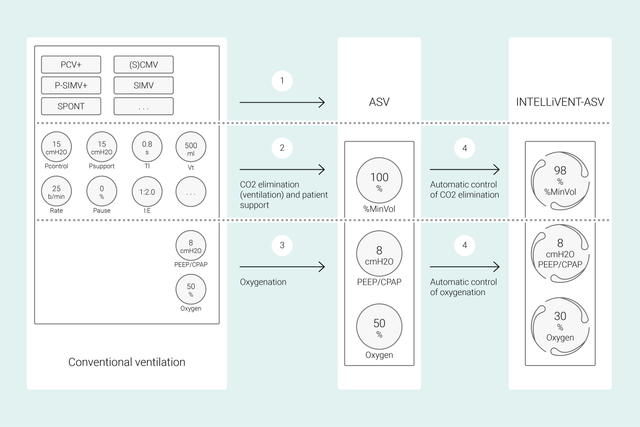
В обычных режимах, чтобы достичь нужных клинических показателей, на аппарате ИВЛ нужно настраивать различные параметры: дыхательный объем или давление, частоту дыхания, FiO2, PEEP, а также время выдоха и вдоха. Кроме того, все эти параметры требуется часто проверять и регулировать.
А при использовании режима INTELLiVENT-ASV главное – определить целевые клинические показатели и стратегии оксигенации и вентиляции. После этого вы можете решить, в какой степени режим INTELLiVENT-ASV будет управлять оксигенацией и вентиляцией, чтобы достичь заданных целей.
Затем режим INTELLiVENT-ASV автоматически выбирает настройки аппарата ИВЛ, управляет переходом между пассивным и активным состояниями и активно поддерживает ваши протоколы отлучения с помощью функции «Быстрое отлучение».
Многочисленные международные исследования продемонстрировали безопасность и эффективность режима INTELLiVENT-ASV в различных клинических сценариях – от перенесенных операций на сердце (


В этом видео старший реаниматолог Жан-Мишель Арналь кратко демонстрирует основные функции и настройки INTELLiVENT-ASV на реальном пациенте отделения интенсивной терапии.
Сначала указываются рост и пол пациента и, при необходимости, особые состояния: ARDS, «Хр. Гиперкап.» или «Повр. мозга». Далее устанавливаются целевые показатели оксигенации (SpO2) и выведения CO2 (PetCO2) для пациента.
После этого доступны различные варианты тонкой настройки режима INTELLiVENT-ASV. Например, можно указать, как будет осуществляться настройка PEEP: вручную либо автоматически в пределах заданного диапазона. После проверки или установки границ тревог все готово к вентиляции.
Режим INTELLiVENT-ASV реализует выбранную вами стратегию лечения. Вместо того чтобы постоянно изменять отдельные настройки, вам достаточно следить за целевыми значениями и стратегией и при необходимости их корректировать.
В режиме INTELLiVENT-ASV значения параметров для пациента устанавливаются и поддерживаются в заданном врачом целевом диапазоне; при этом настройки защиты легких сохраняются (
Эти данные поступают от трех датчиков: проксимальный датчик потока передает сведения о механике легких и активности пациента, а датчики SpO2 и CO2 – об оксигенации и выведении CO2.
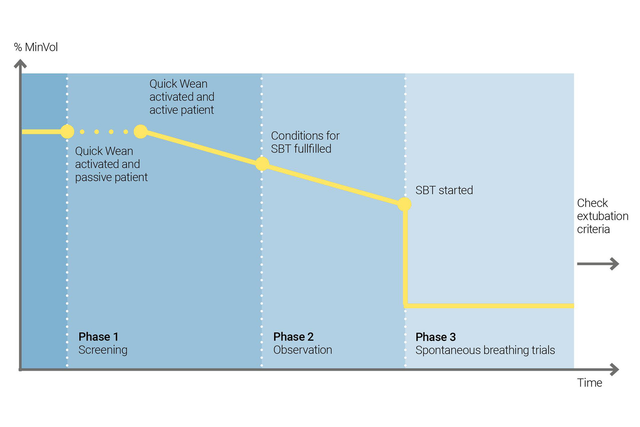
Используйте функцию «Быстрое отлучение» в режиме INTELLiVENT-ASV, чтобы реализовать свой протокол отлучения. Ее можно включить во время вентиляции, если пациент дышит спонтанно.
Чтоб настроить функцию «Быстрое отлучение», следует включить выполнение контролируемых тестов спонтанного дыхания (ТСД). Так вы определите, можно ли отлучать пациента от аппарата ИВЛ. вы задаете критерии для запуска ТСД, настройки, которые будут использоваться во время ТСД, а также критерии для их прерывания.
В режиме INTELLiVENT-ASV всегда отображается история всех выполненных ТСД. Если ТСД выполнить не удается, режим INTELLiVENT-ASV возвращается к предыдущим настройкам вентиляции.
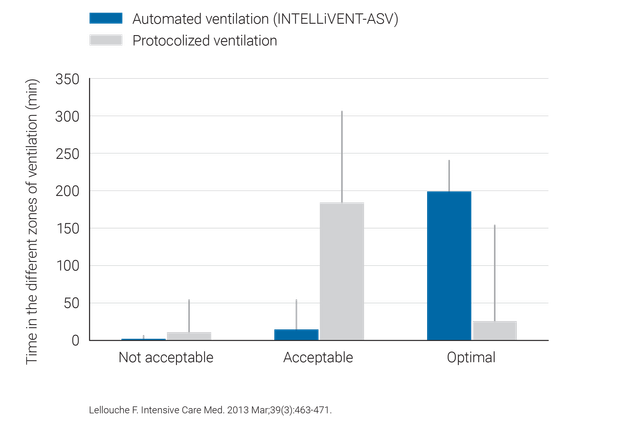
Клинические исследования показали, что режим INTELLiVENT-ASV выбирает безопасное рабочее давление (
Режим INTELLiVENT-ASV требует меньше ручных настроек, чем обычная вентиляция, и, таким образом, помогает снизить нагрузку на медицинский персонал (

Режим INTELLiVENT-ASV доступен как опция в аппаратах ИВЛ HAMILTON-C6, HAMILTON-G5, HAMILTON-C3, HAMILTON-C1 и HAMILTON-T1, а также является стандартным режимом в аппарате HAMILTON-S1.