
Автор: Clinical Experts Group, Hamilton Medical
Дата: 14.12.2017
Last change: 13.07.2020
More information on physiological effects; initial flow setting lowered from 60 to 30High flow oxygen therapy combines several physiologic effects.

The physiologic effects of HFOT are improved oxygenation, reduced inspiratory effort and work of breathing, improved lung mechanics, increased end-expiratory lung volumes (EELV), probably due to the positive end-expiratory pressure (PEEP) effect, increased carbon dioxide (CO2) clearance by washout of anatomic dead space, and improved comfort (
The PEEP effect and the decrease in in respiratory rate are flow-dependent and better with higher flow rates (
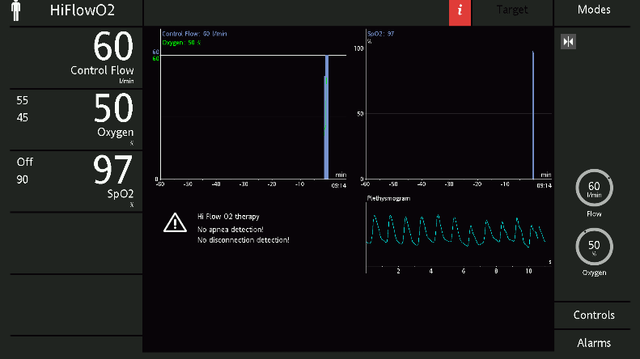
Flow: While many of the targeted physiologic variables show the most benefit at higher flows, patient comfort and compliance to therapy are key factors that should not be ignored. The set flow should take into consideration the severity of the patient’s condition.
Although there is no standard way to set the flow, an approach now used frequently in clinical practice is to initiate with a minimum flow of 30 l/min, and monitor dyspnea and the respiratory rate. If there is no improvement, the flow can be titrated according to patient comfort. You can increase it in increments of 10 l/min up to 60 l/min, and monitor the patient’s clinical condition. Note that any discomfort is usually due to the velocity of gas rather than the flow itself, and may be eased by using a large-bore cannula.
Temperature: In order to optimize the humidification effect, the temperature should be set at 37°C.
Oxygen: Oxygen is adjusted to maintain SpO2 within target ranges of 92%-96% for most patients and 88%-92% for patients with chronic respiratory disease (
This bedside tip is based on the example of high flow oxygen therapy with Hamilton Medical ventilators, however the information applies to the use of high flow oxygen therapy in general.
Full citations below: (

High flow oxygen therapy is available as an option on all our ventilators. We also offer compatible high flow interfaces and a compatible humidifier. In just a few steps, you can change the interface and use the same device and breathing circuit to accommodate your patient’s therapy needs.
We also have some exclusive offers for HFNC enthusiasts where something exciting about high flow nasal cannula therapy is waiting you.
В нашей электронной книге, посвященной терапии с высокой скоростью потока с помощью назальной канюли, описаны ее принцип действия и клинические преимущества, а также приведены практические сведения о выборе правильного интерфейса, настройке параметров и наблюдении за пациентами.