Author: Clinical Experts Group, Hamilton Medical
Date of first publication: 22.02.2018
Optimal patient-ventilator synchrony is of prime importance, as asynchronies lead to increased work of breathing and patient discomfort.
Asynchronies are also associated with higher mortality and prolonged mechanical ventilation (
When trying to synchronize the ventilator with the patient’s activity, there are two main settings to be considered: the inspiratory and the expiratory trigger. These dictate when the ventilator starts or ends a spontaneous breath. On Hamilton Medical ventilators, the setting for the expiratory trigger is the expiratory trigger sensitivity (ETS). This value represents the percent of peak inspiratory flow at which the ventilator cycles from inspiration to exhalation. On Hamilton Medical ventilators, ETS can be set to anywhere between 5% and 80%. In general, increasing the ETS setting results in a shorter inspiratory time, while decreasing it results in a longer inspiratory time.
On other devices, this flow cycle mechanism is called ‘ESENS’, ‘End Inspiration’, ‘Flow Cycle’, etc.
Another criterion for breath termination is TI max. This setting is used if gas leakage is significant and the set cycle is not reached, providing a back-up so that inspiration can be terminated. The ventilator switches over to exhalation when the set TI max is reached.
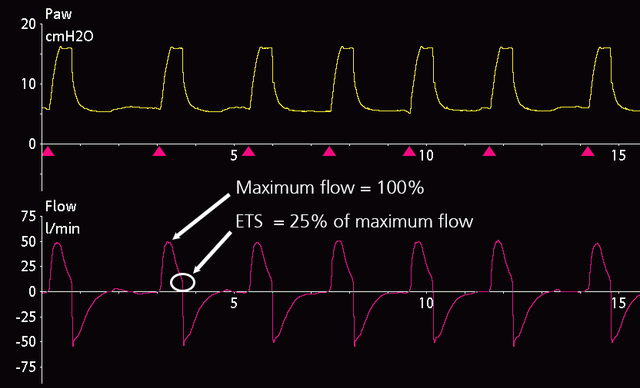
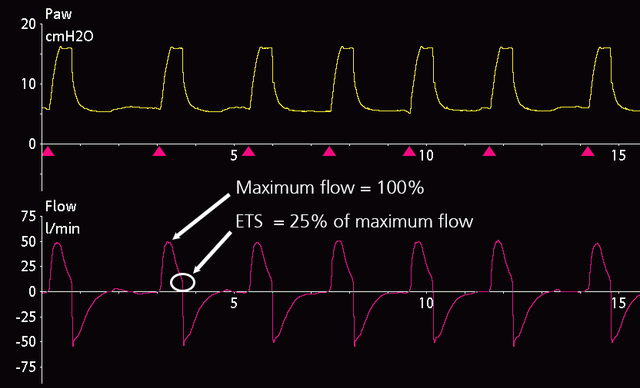
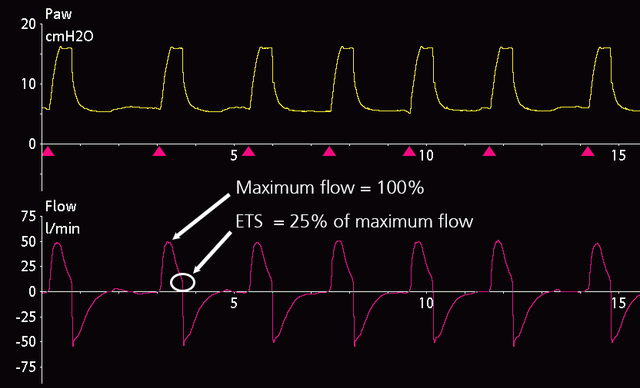
A typical ETS setting in a patient with normal lung mechanics undergoing NIV is 25%, which is the default ETS setting on Hamilton Medical ventilators (see Figure 1). With obstructive patients, for example, in a patient with chronic obstructive pulmonary disease (COPD), ETS should be set higher to increase the expiratory time and thus avoid air-trapping and intrinsic PEEP.
Incorrect ETS settings leading to expiratory asynchrony may be recognized from either delayed or premature cycling leading to double triggering.
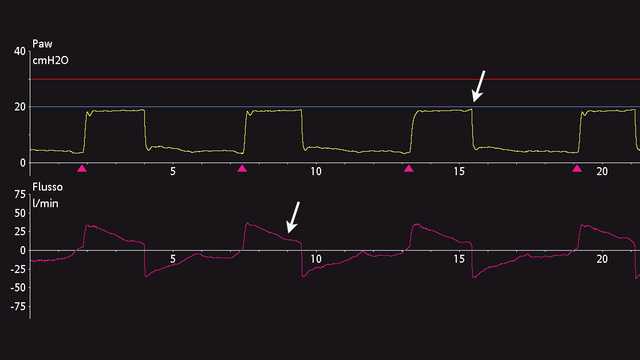
Delayed cycling can be recognized from an end-inspiratory peak in the pressure curve caused by an active expiratory effort, as well as a change in the slope of inspiratory flow towards the baseline (see Figure 2). This is typically described in patients with COPD. The reduction in inspiratory flow is smaller, probably due to dynamic hyperinflation and airway resistance.
In the case of delayed cycling, increase ETS in increments of 10% to shorten the inspiratory time (TI) and adjust TI max according to the patient’s condition.
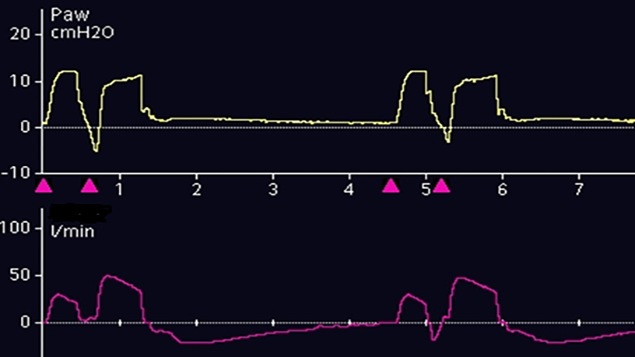
Along with short inspiratory times, double triggering is an indication of premature cycling (see Figure 3). During premature cycling, the inspiratory muscles continue to contract, causing the ventilator to anticipate a second effort. This leads to double triggering, with delivery of higher tidal volumes, breath stacking, and higher work of breathing. A possible solution is trying to match the neural inspiratory time with the ventilator inspiratory time. Double triggering may also be caused by insufficient pressure support.
In the case of double triggering, decrease ETS in increments of 10% to lengthen TI, adjust TI max according to the patient’s condition, or increase Psupport to achieve the desired tidal volumes.
The HAMILTON-C6 and HAMILTON-G5/S1 ventilators offer the option of automatic adjustment with IntelliSync+ (

Our asynchrony reference card gives you an overview of the most common asynchrony types, their causes, and how to detect them.