Die Phasen eines volumetrischen Kapnogramms, die Form und die Kurvenmorphologie sowie die Messungen, die auf den Berechnungen basieren, können Ihnen wichtige Informationen über Folgendes liefern:
Bei unseren Beatmungsgeräten wird das CO2 mit einem CAPNOSTAT-5 Hauptstrom-CO2-Sensor proximal zum Atemweg des Patienten gemessen.
Der CAPNOSTAT-5 Sensor liefert präzise Messungen des endtidalen Kohlendioxids (PetCO2) und ein klares, genaues Kapnogramm bei allen Atemfrequenzen von bis zu 150 Atemzügen pro Minute.
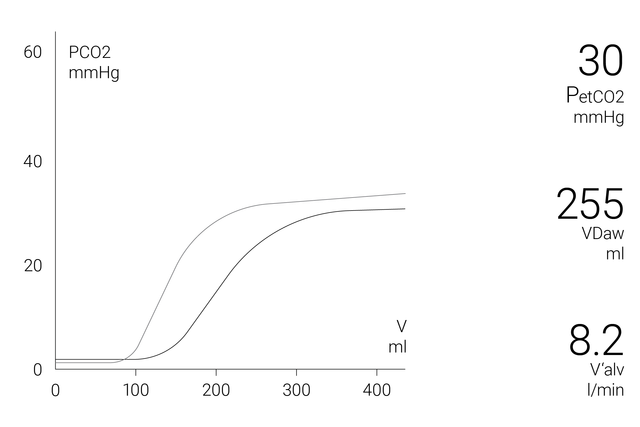
Das volumetrische Kapnogramm-Fenster auf dem Bildschirm zeigt genaue quantitative Informationen als Kombination von proximalen Flow- und proximalen CO2-Daten an, wie z. B.:
Um eine umfassendere Analyse des Patientenzustands zu ermöglichen, steht ein 72-Stunden-Trend (bzw. ein 96-Stunden-Trend beim HAMILTON-G5/S1) für folgende Werte zur Verfügung:
Um Ihnen das Leben zu erleichtern, bieten die Beatmungsgeräte von Hamilton Medical im CO2-Monitoring-Fenster einen Überblick über alle relevanten CO2-bezogenen Werte.
Das eBook erklärt, wie ein volumetrisches Kapnogramm interpretiert wird, und stellt einen Überblick über die Vorteile und klinische Anwendung der volumetrischen Kapnographie zur Verfügung. Selbsttest inkludiert!
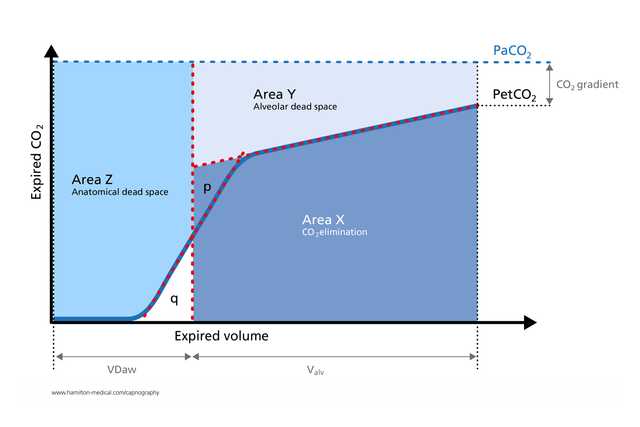
Das volumetrische Kapnogramm wurde erfolgreich für die Messung des anatomischen Totraums, der pulmonalen Kapillardurchblutung und der Beatmungseffizienz eingesetzt (
Die aus der volumetrischen Kapnographie abgeleiteten Berechnungen sind nützlich, um eine Lungenembolie am Patientenbett zu erkennen (
In einer Studie an maschinell beatmeten ARDS-Patienten waren volumetrische Kapnographie-Messungen des Verhältnisses von physiologischem Totraum zu Tidalvolumen ebenso genau wie die Werte, die mit der Überwachung der metabolischen Rate ermittelt wurden (
Das exspiratorische Kapnogramm ist eine anstrengungsunabhängige, schnelle und nichtinvasive Messung, die bei erwachsenen Asthmapatienten die Erkennung signifikanter Bronchospasmen unterstützen kann (
Die volumetrische Kapnographie bietet auf nichtinvasive Weise in Echtzeit wertvolle Einblicke in die Physiologie des Lungenkollapses und des Recruitments und eignet sich daher zur Überwachung zyklischer Recruitmentmanöver am Patientenbett (

Wir bieten Originalverbrauchsmaterialien für Erwachsene, Pädiatrie und Neonaten. Je nach den Richtlinien in Ihrer Einrichtung haben Sie die Wahl zwischen wiederverwendbaren Produkten und Ausführungen für den Einmalgebrauch.
Die volumetrische Kapnographie ist auf den Beatmungsgeräten HAMILTON-C6, HAMILTON-G5, HAMILTON-C3, HAMILTON-C1/T1 als Option verfügbar und gehört auf dem HAMILTON-S1 zu den Standardfunktionen.