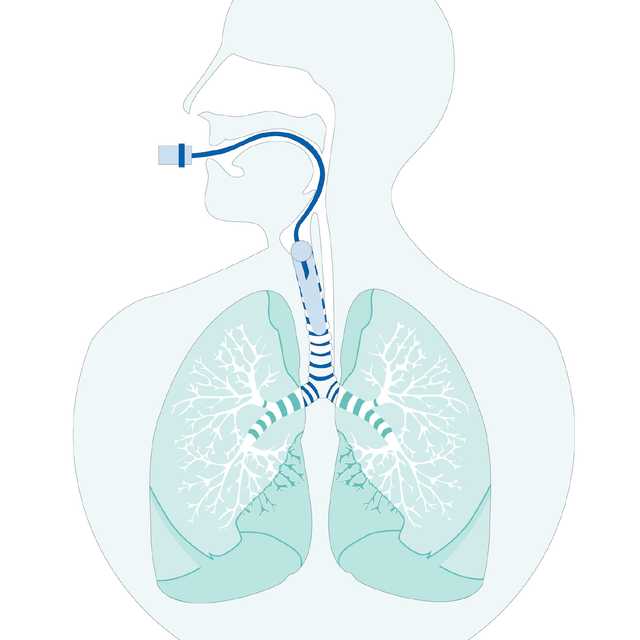
Ein kontinuierlich optimierter und kontrollierter Cuff-Druck unterstützt die Beatmungstherapie und schützt Ihre Patienten vor ventilatorassoziierter Pneumonie (VAP) sowie vor Verletzungen der Trachea (
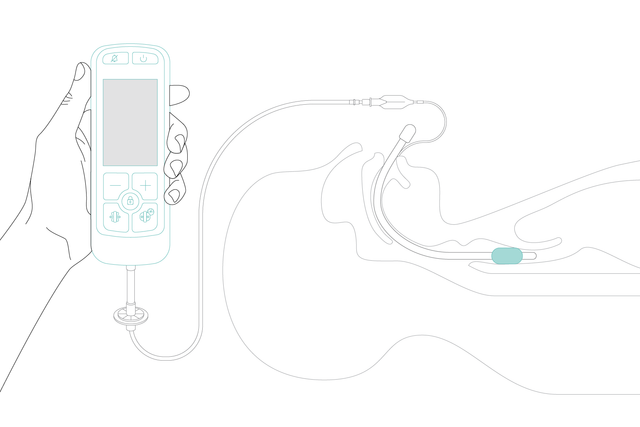
Mit IntelliCuff ist der Grossteil dieser Arbeit für Sie bereits erledigt. Stellen Sie einfach den gewünschten Cuff-Druck ein und IntelliCuff hält ihn automatisch aufrecht. Das Gerät kann innerhalb eines breiten, aber sicheren Druckbereichs für verschiedene Endotrachealtuben mit Cuff arbeiten.
Gleich, ob Sie es für den Lufttransport bei sich schnell änderndem Umgebungsdruck oder im Operationssaal während einer N2O-Narkose oder einer Operation verwenden, IntelliCuff überwacht kontinuierlich den optimalen Cuff-Druck und hält ihn aufrecht, um die Patientensicherheit zu erhöhen. Selbst in den kritischsten Situationen (


Geeignet für erwachsene, pädiatrische und neonatale Patienten. IntelliCuff sichert das Atemwegsmanagement in verschiedenen Situationen – auf der Intensivstation, im Operationssaal oder beim Transport. Sie können es für die Notfallrettung an Land oder in der Luft verwenden – auch in grösseren Höhen.

Wir setzen IntelliCuff bei maschinell beatmeten Patienten als Standardfunktion ein, um VAP zu vermeiden. IntelliCuff kontrolliert den Cuff-Druck automatisch und regelmässig. Das ist eine grosse Hilfe für uns Pflegekräfte, da wir den Druck nicht jede Stunde manuell überprüfen müssen.
Stationsleiterin Intensivpflege
Kantonsspital Graubünden, Chur, Schweiz




Verschiedene Schnittstellen ermöglichen es Ihnen, den IntelliCuff genau dort zu befestigen, wo Sie ihn benötigen. Mit nur einem Klick.


Das eigenständige IntelliCuff Gerät ist der perfekte Begleiter für die Beatmungsgeräte von Hamilton Medical.