Der proximale Flow-Sensor ist seit 1983 das Herzstück unserer Beatmungsgeräte. Der gesamte Beatmungsprozess hängt von der Messung und Genauigkeit des Flow-Sensors ab, der auch Daten von der Atemwegsöffnung liefert.
Präzise Volumen-, Flow- und Druckdaten sind entscheidend für eine korrekte Diagnose und die Vermeidung von häufigen Nebenwirkungen aufgrund ungeeigneter Beatmungseinstellungen. Sie ermöglichen auch die Anwendung einiger unserer hochmodernen Technologien, wie z. B. die Modi ASV und INTELLiVENT-ASV, IntelliSync+ und das P/V-Tool.

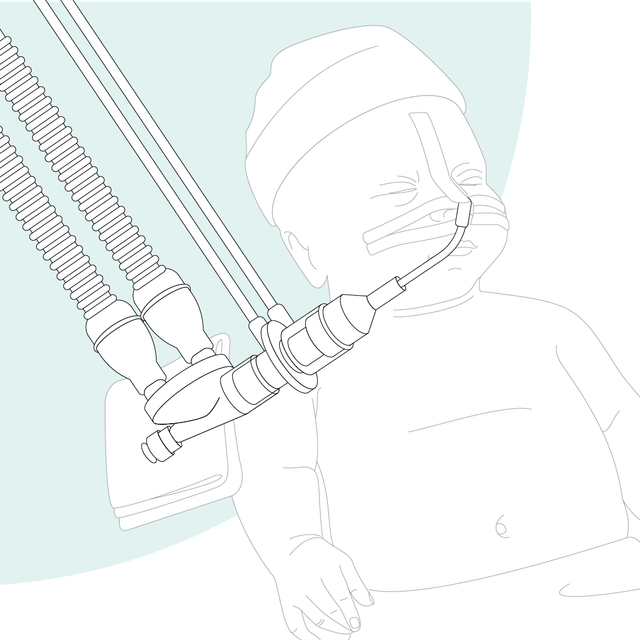
Unsere Beatmungsgeräte messen Flow und Druck nahe am Atemweg des Patienten. Studien haben gezeigt, dass die Tidalvolumina für beatmete Patienten mit einem am Endotrachealtubus platzierten Flow-Sensor bestimmt werden sollten (

Die genaue Bestimmung des ausgeatmeten Tidalvolumens (VTE) ist von entscheidender Bedeutung (
Ihre Vorteile:
Wir bieten Verbrauchsmaterialien von Hamilton Medical für erwachsene, pädiatrische und neonatale Patienten. Je nach den Richtlinien in Ihrer Einrichtung haben Sie die Wahl zwischen wiederverwendbaren Produkten und Ausführungen für den Einmalgebrauch.
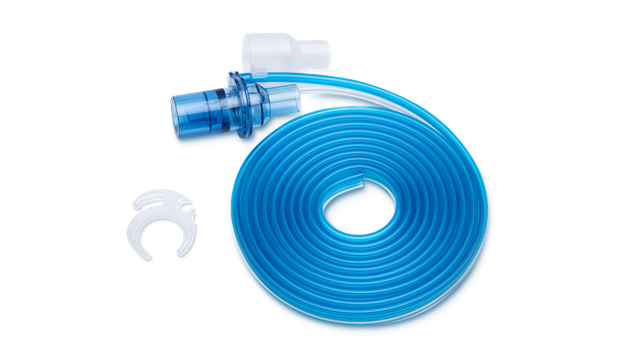

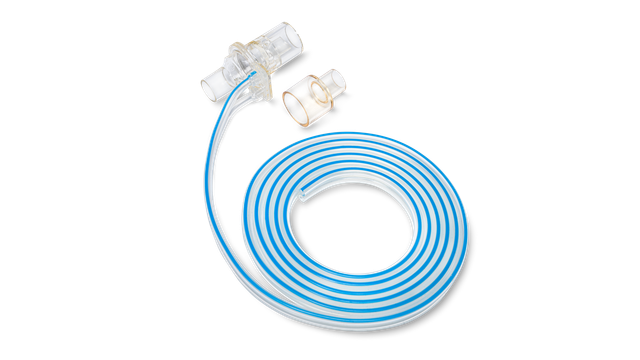

Mit den Flow-Sensoren für den Einmalgebrauch von Hamilton Medical müssen wir uns keine Gedanken mehr zu einer Kreuzkontamination machen, da wir denselben Flow-Sensor nicht bei einem anderen Patienten einsetzen.
Leiter der Beatmungsstation bis 2018
University Medical Center, Lubbock (TX), USA